Rinderpest, or cattle plague, is an acute, highly contagious viral disease of wild and domesticated ruminants and pigs. It is characterized by sudden onset of fever, oculonasal discharges, necrotic stomatitis, gastroenteritis and death.
In a fully susceptible population, as is the case in non-endemic areas, morbidity and mortality can approach 100 percent. With some strains of the virus, however, the disease may be mild with low mortality from infection.
Formerly widespread throughout Europe, Asia and Africa, rinderpest has now been limited to fairly well-defined locations in South Asia, the Near East and eastern Africa. This has been achieved through various national and regional rinderpest eradication programmes. Global rinderpest eradication, which is being targeted for 2010, is being coordinated by FAO.
Rinderpest virus belongs to the morbillivirus genus of the paramyxovirus family. Other members of the genus include the measles virus of humans, the peste des petits ruminants virus of domesticated and some small wild ruminants, the canine distemper virus of dogs and wild carnivores and the morbilliviruses of aquatic mammals.
There is only one serotype of rinderpest virus, but the different strains vary in their pathogenicity.
Susceptible species
Large domestic ruminants. Although all cloven-hoofed animals are probably suceptible to infection, severe disease occurs most commonly in cattle, domesticated water buffaloes and yaks. Breeds of cattle differ in their clinical response to rinderpest virus. Some breeds have developed a high innate resistance through selection by long association with the disease.
Sheep and goats are generally less susceptible but may develop clinical disease.
Asiatic pigs are susceptible and may suffer clinical disease. European breeds are less susceptible. The latter tend to undergo subclinical infection and play little or no part in the maintenance of the disease.
Camels are apparently not infected and appear to have no role in rinderpest transmission and maintenance.
Wildlife. Some species, such as African buffalo, eland, giraffe, lesser kudu and warthog and Asian antelopes, bovids and swine, are highly susceptible. Others, such as antelopes, hippopotamus and Indian blackbuck are less susceptible. There is no evidence to suggest that wildlife populations can maintain the disease indefinitely without concurrent disease in cattle.
Rinderpest does not infect humans.
Transmission
Almost invariably, rinderpest spreads between herds and to new areas by the movement of infected animals. Infected cattle start shedding virus one or two days before the appearance of clinical signs. They continue to shed virus for about nine to ten days after the onset of fever, and generally harbour the virus for no more than three weeks. Infected cattle may spread virus through markets and transport it long distances before clinical evidence of the disease is observed.
Rinderpest virus is found in expired air, nasal and ocular discharges, saliva, faeces, milk, semen, vaginal discharge and urine. Infection is transmitted primarily by inhalation of expired air contaminated by infected droplets or by contact with secretions and excretions from infected animals. Transmission occurs mainly over short distances, but occasionally may occur over distances of up to 100 m or more at night, when the effects of high temperature and sunlight are minimal, especially in conditions of very high humidity.
Transmission through the oral route by ingestion of contaminated feed and water is possible. Infected meat stored at 4°C can remain inefective for at least seven days. Feeding of infected meat and feed contaminated with infective secretions and excretions may serve as a source of infection for pigs, which may then transmit the disease to cattle.
Rinderpest is not transmitted by insect vectors.
Virus stability
At 4°C, rinderpest virus is most stable at pH values of 7.2 to 7.9 and is rapidly inactivated at pH less than 5.6 or greater than 9.6. The virus is inactivated rapidly at environmental temperatures by solar radiation and desiccation. Pasture is infective for six hours if unshaded or 18 to 48 hours if shaded. Contaminated bare enclosures are infective to cattle for no more than 48 hours and contaminated buildings for a maximum of 96 hours.
The virus is highly susceptible to many lipidsolvent disinfectants because it is enveloped. It is also susceptible to both acid and alkaline conditions. It is inactivated rapidly by autolysis and putrefaction and hence does not survive for more than 24 hours in the carcass of an animal that has died from the disease.
The virus is present in milk one or two days before appearance of clinical signs. Heat treatment or pasteurization of milk is sufficient to inactivate the virus.
DOMESTICATED
WATER BUFFALOES
The national
rinderpest
contingency plan
should include
provisions for this
species, as the
disease is commonly
seen in buffaloes
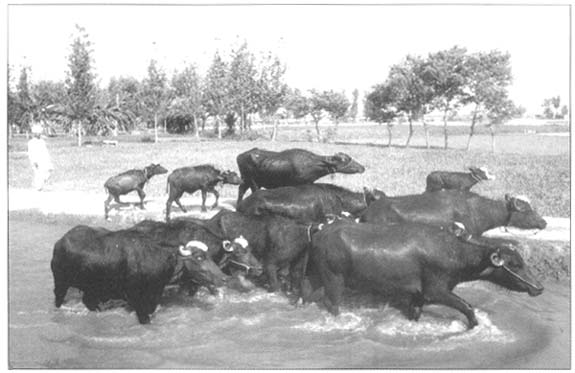
Cattle
Rinderpest is capable, in certain situations, of causing devastating losses in cattle herds, but tends to have less impact in endemic areas and on partially immune populations. The disease may be peracute, acute or mild, depending on a number of factors inherent in the virus strain, the host and the system of management of the animals.
Peracute rinderpest. In peracute rinderpest, there is a sudden onset of fever, inappetence, depression, congestion of the visible mucous membranes and death within two to three days, before oral erosions develop.
Acute rinderpest. The OIE International animal health code puts the incubation period of rinderpest as 21 days for purposes of zoosanitary measures. The route of infection, the dose and the virulence of the strain of virus may modify the incubation period. In general, the period between the first index case and the appearance of secondary cases is about two weeks.
Typically, the disease is heralded by a sudden onset of pyrexia, which may last anything from between three and five days to two weeks, before returning to normal. This is accompanied by restlessness, depression, inappetence and a significant fall in milk yield. Respirations are shallow and rapid. One or two days later, serous oculonasal discharges and severe congestion of the mucous membranes of the eyes and nose are typically seen.
Two to five days after the onset of fever, tiny, pinpoint greyish areas of necrosis appear on the gum and lips. The lesions increase in number, enlarge and coalesce to form a thick, yellow pseudo-membrane covering the oral mucosa including the lateral and ventral aspects of the tongue. The necrotic debris easily desquamates, leaving shallow erosions with red layers of basal cells. Similar erosions can also be seen on the mucous membranes of the nose, the vulva and the vagina. Salivation is stimulated, the saliva being initially mucoid and then mucopurulent. A distinctive foul odour exudes from the mouth.
Diarrhoea starts one to three days after the appearance of oral lesions. The faeces are initially thin and dark in colour, and may later become watery and contain mucus, shreds of epithelium and specks of clotted blood. Occasionally the liquid faeces may be red in colour. Affected animals arch their backs and strain, sometimes exposing congested and eroded rectal mucosae.
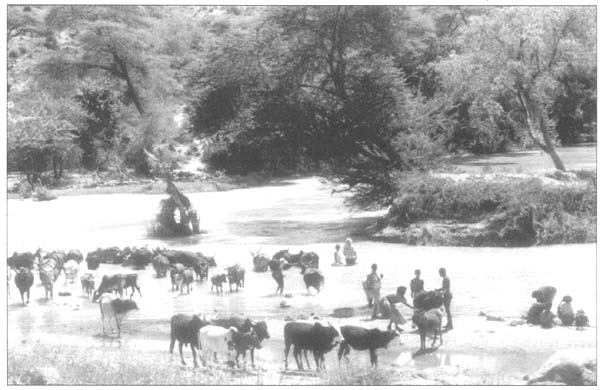
A COMMON
WATERING-POINT
Rinderpest
transmission and
spread are enhanced
by congregation of
different herds of
animals, as occurs at
common watering-points
Respirations are laboured and painful and there may be an audible grunt on expiration. In fatal cases the diarrhoea continues to worsen, causing rapid dehydration and visible wasting. Sternal recumbency follows and death supervenes 6 to 12 days after the onset of fever. If animals survive, the erosions heal, diarrhoea stops and a prolonged convalescence follows, with recovery to full health taking many weeks. Pregnant cows commonly abort in the convalescent period.
Skin lesions, which appear as a maculopapular rash on the less hairy parts of the body such as the groin and axillae, have been described.
Mild rinderpest. The evolution and clinical signs of mild rinderpest are similar to those of the classic syndrome but are less marked. One or more of the cardinal features may be absent or only present transiently, particularly oral erosions, which may be meagre. Most affected cattle recover, and convalescence is short. A frequent sequel of mild infections is activation of latent pathogens, notably protozoa, occurring four to six days after the start of the prodromal fever. The signs of the activated infection may predominate and mask the appearance of clinical signs of rinderpest.
Sheep and goats
Small ruminants more commonly suffer the subacute form of the disease, characterized by transient fever without remarkable systemic disturbances. In areas where peste des petits ruminants (PPR) is endemic, most rinderpest-like syndromes are more likely to be PPR. However, acute rinderpest can occasionally be seen in small ruminants. Clinical manifestations are similar to those seen in cattle, and consist of fever (rectal temperatures of 41 to 42°C), focal to coalescent necrotic stomatitis, oculonasal discharges, conjunctivitis, pneumonia and diarrhoea.
Pigs
Asiatic breeds of pigs may suffer peracute or acute rinderpest. Peracute disease is characterized by sudden onset of fever and death without further premonitory signs. Acute disease in these breeds of pigs is manifested by sudden onset of fever, inappetence, depression, shivering, vomiting and epistaxis. Shallow erosions, diarrhoea, progressive but rapid dehydration and emaciation precede death.
MILD RINDERPEST IN CATTLE
One or more of the cardinal features may be absent or
only present transiently, and affected animals may not
look overtly sick
Wildlife
Wild ungulates differ markedly in their manifestation of rinderpest infection. Buffaloes react with a clinical syndrome essentially the same as that in cattle, whereas lesser kudus exhibit profuse discharge of tears and corneal opacity progressing to death from dehydration and starvation. Any unexplained incidence of morbidity and mortality in wild ungulates in areas where there is a risk of rinderpest should be viewed with suspicion and investigated thoroughly. Generally, strains of rinderpest virus that produce mild disease in cattle may cause severe disease in susceptible wildlife species.
Gross pathology
The carcass is dehydrated, sometimes emaciated and soiled with loose faeces. The eyeballs are sunken and encrusted with mucopurulent discharges. The muzzle and external nares may be encrusted with similar exudates.
The oral cavity usually contains necrotic material and areas of erosion from desquamated epithelium, primarily on the gums, buccal papillae, lateral and ventral aspects of the tongue and the soft palate. In severe cases, these erosions extend to the pharynx, the oesophagus and the forestomach. Lesions consisting of congestion, oedema, haemorrhages and erosions may also be seen in the abomasum and the small intestines.
The large intestines, from the caecum to the rectum, may show varying degrees of congestion, erosions and linear haemorrhages (usually described as zebra striping), especially around the ileo-caecal valve and the caecal tonsils. These haemorrhages are bright red in fresh carcasses or greenish-black in stale or decomposing ones.
The mucosa of the upper respiratory tract may be congested and show haemorrhages. The lungs may be normal in animals that died in the early stages of the disease or show congestion and interlobular and alveolar emphysema in older cases.
The lymph nodes in early deaths may be swollen and oedematous but in late deaths may be shrunken and grey, with radial streaks in the cortex. The spleen is usually normal but occasionally may have subserosal haemorrhages along its margins.
Histopathology
Microscopic findings consist essentially of extensive lymphocytolysis with depletion of the lymphocytes in the germinal centres of lymph nodes and the spleen. The epithelial cells of the alimentary tract reveal areas of necrosis and ulceration with formation of multinucleated giant cells as well as intranuclear and intracytoplasmic inclusion bodies in lymphatic cells and alimentary tract epithelial cells.
There is only one immunogenic type of rinderpest virus and immunity to one strain will protect against all other known strains. One vaccine will thus protect against all field strains. Serum antibodies are first detectable within one week of infection with classical rinderpest strains. However, animals infected with mild strains may take ten days or longer to develop neutralizing antibodies, as do animals vaccinated with tissue-culture rinderpest vaccine (TCRV). For all practical purposes, animals are immune one week after vaccination, although serum antibody titres do not peak for about three weeks. Serum neutralizing antibodies are a major component of active immunity against infection and have an important role in recovery.
In endemic areas and those where vaccination is routinely carried out, calves acquire passive immunity with the intake of colostrum from their immune dams and the antibody can persist for up to 11 months, preventing vaccine virus from generating an immune response.
Field diagnosis
Rinderpest should be suspected when there is any unusual occurrence of morbidity associated with a stomatitis-enteritis syndrome characterized by nasal and ocular discharge with any two of the following signs: fever, oral erosions or lesions, excessive salivation, diarrhoea and death. The mild form of rinderpest causes the most difficulty, as one or more of the characteristic features may be missing from the syndrome observed. Lesions may be limited to ocular discharge with only a fleeting appearance of limited oral lesions in a small proportion of affected calves. Only the younger age groups may be affected, the morbidity rate may be low even in them and the mortality rate may be so low as to be indistinguishable from expected mortality in these age groups.
Differential diagnosis
Epidemiological features, as well as clinical and pathological signs, are highly suggestive of rinderpest. However, clinical signs of rinderpest may be similar to those seen in other diseases in which fever, oculonasal discharges, stomatitis and/ or diarrhoea may be prominent features. These include fatal mucosal disease (MD) syndrome of the bovine virus diarrhoea disease (BVD) complex, some forms of malignant catarrhal fever (MCF), foot-and-mouth disease (FMD), peste des petits ruminants (PPR), infectious bovine rhinotracheitis (IBR) and bovine papular stomatitis (BPS). Other diseases that need to be considered in the differential diagnosis of rinderpest are contagious bovine pleuropneumonia (CBPP) and East Coast fever (ECF). Epidemiological features and laboratory diagnostic tests are important in distinguishing between these diseases.
Bovine malignant catarrhal fever. Although rinderpest and BMCF resemble each other in their clinical and pathological features, morbidity rates are generally lower in BMCF. Bilateral, centripetal corneal opacity, accompanied by blepharospasm, photophobia and hypopyon, is a feature only of BMCF. However, corneal opacity is also commonly associated with rinderpest in some wildlife species, especially lesser kudu. Diagnosis is confirmed by polymerase chain reaction (PCR) or histopathology.
Foot-and-mouth disease. FMD can be distinguished from rinderpest by the presence of lameness and by the low mortality and vesicular stomatitis in FMD as opposed to the necrotic stomatitis seen in rinderpest. Diarrhoea, which is commonly a prominent sign of rinderpest, is not a feature of FMD. Diagnosis is confirmed by virus isolation and/or antigen detection.
Mucosal disease/bovine virus diarrhoea. BVD, usually an inapparent to relatively mild disease syndrome lasting a few days, may be seen in cattle at any age, but particularly in calves. Morbidity is usually high but mortality is generally low. MD, on the other hand, is a severe disease of young, growing cattle in which few animals may be affected but, invariably, fatally. Differentiation of MD from rinderpest is achieved by laboratory tests, including virus isolation, immunofluorescence staining, PCR, antigen detection or detection of rising antibody titres.
Infectious bovine rhinotracheitis. This disease may be confused with rinderpest when diarrhoea is not a prominent feature of the latter. Otherwise, the disease caused by the IBR virus is characterized essentially by upper respiratory symptoms. Mortality rates are lower than in rinderpest. It is confirmed by virus isolation and/or antigen detection.
Contagious bovine pleuropneumonia. Diarrhoea, oral necrosis and erosions are not seen in CBPP. The evolution of clinical disease is more protracted in CBPP because of the longer incubation period. Severe emaciation, exercise intolerance and moist, suppressed coughs are features of CBPP. Lung lesions are characteristic.
East Coast fever. The presence of the tick vector and absence of effective tick control, when considered together with other clinical signs and the results of microscopic examination of blood and lymphoid tissues, are useful in the differentiation of ECF from rinderpest.
Laboratory diagnosis
Diagnostic procedures for rinderpest and detailed instructions on collection, preservation and dispatch of samples are contained in the FAO Manual on collection and submission of diagnostic specimens to the World Reference Laboratory for Rinderpest, the FAO Manual on the diagnosis of rinderpest and the OIE Manual of standards for diagnostic tests and vaccines.
Laboratory confirmation of a presumptive diagnosis of rinderpest may be achieved by tests designed to detect live virus, virus antigen, virus genetic materials or antibodies against the virus (in unvaccinated animals).
Collection and transport of diagnostic specimens. Preferred samples for virus isolation are:
For the detection of virus antigen, ocular secretions, necrotic gum debris and samples of the spleen, lymph nodes and tonsils should be collected.
Virus shedding in secretions and excretions starts towards the end of the incubation period before the appearance of clinical signs. It peaks during the febrile/mucosal erosion phase and then declines and stops early in the convalescent period.
Samples are best collected from animals that are febrile and have mucosal erosions and clear lacrymal secretions. It is generally better to collect samples from as many animals as possible to maximize the chances of positive results.
Two sets of tissue samples should be collected, one chilled and the other fixed in formol-saline. Those for virus isolation should be preserved in transport medium (phosphate buffered saline, pH 7.6) with antibiotics and antifungals but without glycerol, which kills the virus.
Samples for virus isolation should be transported to the laboratory as quickly as possible, chilled but not frozen. If storage is imperative for a period of time, samples should be kept at -70°C (not -20°C).
Whole blood (without anticoagulants) should be collected and centrifuged after clotting to obtain the serum needed for virus antibody detection. Serum should be stored at 4°C for short-term or -20°C for longer-term storage.
Each sample should be put in a strong watertight primary container which is then wrapped in absorbent material, placed in a strong leakproof secondary container and then into a solid outer covering. This should be labelled with waterproof ink for dispatch to the national diagnostic, regional and/or world reference laboratories. Information about the carrier, airway bill number and flight time should be sent to the laboratory ahead of dispatch.
Virus isolation. Isolation of virus from lymphoid tissues or blood leucocytes is done in cell cultures and is essential for subsequent virus characterization and molecular epidemiological studies. However, the technique requires trained expertise and aseptic tissue culture facilities, and therefore can only be carried out in well-equipped national and specialized regional and world reference laboratories.
Antigen detection. Three techniques widely used for rinderpest antigen detection and prescribed by the OIE Manual of standards for diagnostic tests and vaccines are the agar-gel immunodiffusion test (AGID), the counterimmunoelectrophoresis (CIE) and the immunocapture enzyme-linked immunosorbent assay (ICE).
AGID and CIE detect precipitating antigens in excretions, secretions and tissue samples. ICE may be used for definitive diagnosis and the differentiation of rinderpest from PPR.
Other techniques that may be used for antigen detection include immunohistochemical staining, immunofluorescence, electron microscopy and a pen-side, monoclonal antibodybased, latex particle agglutination test which is still under evaluation for field use.
Detection of virus genetic material. Rinderpest virus genetic material can be detected by reverse transcription polymerase chain reaction (RT-PCR), which is a very specific and sensitive technique that requires specialist expertise and equipment. This technique is carried out in the collaborating centres and world reference laboratories and in national laboratories that have the required expertise and facilities. Nucleotide sequencing provides phylogenetic information of epidemiological significance.
Antibody detection. A monoclonal antibody-based and specific competitive enzyme-linked immunosorbent assay (ELISA) is widely used and has largely replaced the virus neutralization test for rinderpest antibody detection. This is robust test but it cannot differentiate antibodies caused by vaccination from those caused by field virus.
A risk assessment of possible introduction of rinderpest into the country is essential for formulating a national policy for rinderpest control and elimination. The main risk factors to be considered include:
A statement about the risk profile should be made expressing the probability as extreme, high, medium or low, based on the perceived socio-economic consequences of rinderpest incursion into the country such as:
It is necessary to identify measures that would be needed to reduce these risks, such as a ban on importation of live susceptible animals from high-risk areas, and border quarantine and control.