This guide is for everyone who wants to improve the feeding and nutrition of families in developing countries. It is for you if you are a health worker, nutritionist, agricultural extension worker or any other kind of development worker. It is for you if you are a member of a community group or a mother or other caregiver who wants to know more about family feeding. It might also be useful to anyone training health staff and community workers.
If you do not have a basic knowledge of nutrition and feel uncomfortable dealing with some technical parts of the guide, we suggest that you team up with local professionals so they can give you help when you need it.
The purpose of the guide is to:
provide the information needed to prepare good, nutritious and safe meals and feed each member of the family well;
motivate people to adopt healthy eating habits.
The guide is divided into 11 topics that cover basic nutrition, family food security, meal planning, food hygiene and the special feeding needs of children, women and men, and of old, sick and malnourished people. Each Topic is set out in the same way and has two parts: Nutrition notes and Sharing this information.
The Nutrition notes summarizes up-to-date knowledge on each topic. These can be used to prepare:
face-to-face education sessions with families and other community-level groups (including teachers, care workers, traditional health workers, etc.);
nutrition education print materials (such as booklets, brochures, flyers, posters) or material for other media (such as radio talks);
training materials for different levels of staff in different sectors who deal with family nutrition.
You may also find them useful to update your own and perhaps your colleagues’ nutrition knowledge.
Sharing the information is for people working directly with families and community groups. It describes the steps needed to prepare an education session. These steps are: finding out the community’s present nutritional situation and knowledge; deciding what information to share and with whom to share it; and choosing communication methods. This part also gives some Examples of questions to start a discussion which may help to encourage participation and make the session more fun.
Key messages appear throughout the Nutrition notes and summarize important points being made in the text.You may use them as ‘talking points’ or guidelines for structuring a nutrition education session.
The book contains a glossary and three appendixes covering sources of nutrients in foods, energy and nutrient needs, and additional sources of information.
|
Before using the guide, it is important to adapt the nutrition information to the local area where it will be used.We suggest how to do this in Section B. |
Diets and eating habits vary from place to place. Families in different areas eat different foods and cook in a variety of ways. They live in different regions where the type and amount of food available can differ considerably. They have different beliefs about foods and how to feed their children. The amount of money, time and other resources they have varies and this affects what they eat. Families differ in what they know about nutrition and they obtain information about nutrition in different ways. Since this guide is written in a ‘general’ manner and does not reflect a specific country, part of its technical information will always need to be adapted so that it is suitable for the areas where it will be used. This will also enrich the guide with local knowledge and experiences. Such adaptation can be seen as regular preparation for the use of the guide and specific guidelines for this process are given below.
Some countries or regions may decide to produce a local (national) version of the guide to make it more focused on their specific situation, regarding food and nutrition problems, type of local foods and eating habits, etc. This will help their national health workers and other users to make good and easy use of the guide. Guidelines for this more thorough process of adaptation, which will result in a new, local version of the guide (or similar materials) are also given below.
1. Read the guide. Check the Nutrition notes in each topic. Do you understand and agree with the information given? Recent nutrition research means that some of the data may be different from those you have learned before. Consult your supervisor if necessary.You may want to include some information, or change the names of foods, etc., to make the guide suitable for the communities with which you work.
2. Decide, with colleagues, which of the topics are relevant to the local families. This depends on the nutrition problems in your area and whom they affect.You may want to find answers to the following questions. Are many babies born with a low birthweight? Are many babies not exclusively breastfed? Are poor feeding practices of children or women a problem? Are old or sick people fed poorly? Is anaemia a problem and who is most affected? Are many people overweight? What are the nutritional and other causes of these disorders? Do people living with HIV/AIDS know which foods help them to stay well? What nutrition information do groups and families request themselves?
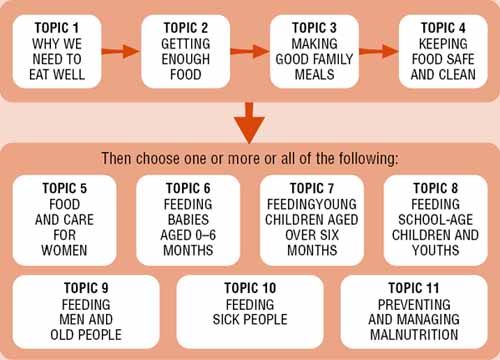
3. Select the topic(s) you want to share and decide how to do this. Unless you are sure that people understand the basic facts of healthy nutrition, you should try to include Topics 1, 2, 3 and 4 in any nutrition education (or training) course. Box 1 suggests a good order in which to use the Topics. Suggestions for how to select the Topics in different situations are given in the following examples.
You may be working with a group or family on several occasions. For example, you may be making several visits to a youth or religious group or you may be working with mothers and caregivers who regularly come to a young child or antenatal clinic, or to community growth monitoring sessions. In this case, you may have sufficient time to follow the order suggested in Box 1. If you have time to cover only a few topics, start with Topic 1 to ‘set the scene’ and then choose only those topics that are relevant to and/or requested by the group or family.
You may be invited by a group of women or farmers to talk about one specific topic, such as feeding children. In this case you may need to use parts of Topic 1 (Why we need to eat well), Topic 3 (Making good family meals) and/or Topic 4 (Keeping food safe and clean) so that participants understand the basics of nutrition, meal planning and hygiene. Then use Topic 6, 7 or 8, each of which discusses in full about feeding children of different ages.
You may be visiting the home of a malnourished child. This gives you a chance to assess the particular educational (as well as other) needs of the family. You may need to use parts of Topic 1 (if you think the mother or other caregiver needs a reminder of ‘basic nutrition’) and perhaps Topic 4 (if poor hygiene is a problem) and then Topic 11 and - depending on the child’s age - Topic 7 or 8.
BOX 1 · SUGGESTED ORDER FOR SHARING THE TOPICS
4. Select information from the Nutrition notes that is relevant and practical for the particular group or family. Do not try to cover too much at one time. It is better to share a small amount of relevant information than to cover all the material in the Topic. Adapt the information and advice to the situation and resources of the group or family (e.g. suggest local foods that a family can produce or buy; demonstrate recipes using local stoves and fuel; use local words for disorders such as anaemia).
5. Select the method for sharing the information. This depends on whom you are trying to reach. Some examples are the following.
Group discussions. These are useful at clinics and meetings of community groups, such as women’s, youth, farmers’ and religious groups. Box 2 explains how to use questions to encourage participation and make the discussion livelier.
Counselling of individuals or families. This can be done in private, at clinics, in maternity units or in homes. Counselling is a dialogue between you and another person (e.g. a mother, a father) which helps the person make informed decisions about her/his future behaviour.
Demonstrations (see Figure 1, page 6). Demonstrations are useful to show how to prepare a meal or snack, how to keep food hygienically and how to feed a young child or sick person.
Personal example. In most communities there are people who, in spite of limited resources, are feeding their families successfully. A good way to persuade other families to improve food and feeding practices is to ask these successful people to share information about what they are doing. For example, mothers who exclusively breastfeed can talk with pregnant women; families with healthy young children might explain how they sit with their children at meals and encourage them to eat; schools with successful gardens can share knowledge of gardening methods with other schools; women’s groups can share recipes for preserving foods.
Songs, poems and drama. Use these to introduce a topic or reinforce messages
6. Find the blocks that may prevent families from improving their feeding practices. These may be: lack of resources (such as money, women’s time); existing beliefs, traditions and food taboos; pressures from other family members, particularly men; unavailability of foods or agricultural inputs; inappropriate or culturally insensitive advice. If an individual or family is not feeding as recommended, find out why. There may be many reasons and you may have to probe sensitively to discover them (e.g. the family may be embarrassed by lack of money; a mother is not breastfeeding because she fears she is HIV+). Then discuss together what a family is able and willing to do. It may be best to first encourage a small, easy change in behaviour. A family may agree to make a small change but not a big one. For example, a mother may agree to spend more time feeding a young child but would not be able to give the child an extra meal a day. Discussions with other family members may help a mother make a change. Perhaps the family can do some of the mother’s work so she has more time to feed a sick child.
BOX 2 · DISCUSSION GROUPS - HOW TO ENCOURAGE PARTICIPATION
|
One way to make a discussion more interesting and effective is to ask questions instead of telling people what to do. Asking questions allows you to find out what people already know and believe. It makes people take an active part and discuss together traditional beliefs and new concepts. It is more likely to lead eventually to small or large changes in behaviour. Example of the start of a discussion on feeding during pregnancy (see Topic 5) Situation: A meeting of a women’s group in a rural area of Africa. The group identified the problem that some women do not eat extra food during pregnancy. You, a nurse, have been invited to the meeting to lead the discussion. Here are some questions that you can use to stimulate participation. You may need to encourage some people, especially shy or young women, to take part. You may have to prevent one or two people from dominating the meeting. Remember to be very polite. Never tell anyone they are ‘wrong’ but emphasize ‘correct’ responses and beliefs. Aim to get a group to agree to make at least a small change to improve any poor feeding practices. Ask: “Thank you for inviting me to this meeting so we can discuss together how to eat well during pregnancy. First, let me ask, should we eat more or less food when we are pregnant?” Wait for a few responses. Then say, “I agree with those of you who said ‘more’, it is important to eat more during pregnancy”. Ask: “Why do pregnant women need extra food?” Agree with correct responses: for example, “We need extra food to build the placenta and the baby’s body”. Add other reasons if they are not mentioned. Gently correct ‘wrong’ answers if necessary. Explain that women who do not eat enough are likely to have small, weak babies. Ask: “How can pregnant women increase their food intake during pregnancy?” Responses could include ‘eating more often’ or ‘eating more at each meal’. Describe or show an example of the amount of extra local foods needed. Ask: “Are there any foods that are especially good for pregnant women?” Allow several responses and catch ‘correct’ ones (e.g. iron-rich foods, such as beef or liver). Continue asking questions and ‘catching’ and explaining correct answers. Give people plenty of opportunity to ask you questions. At the end say, “Are there any other questions? Thank you. I have learned a lot from you today”. |
7. Evaluate your work. The purpose of the guide is to help families improve feeding practices. You may want to interview families or groups to ask what information they found useful, what they learned that was new and what they have put into practice. When you see an individual family again, find out if they have made any of the suggested behavioural changes. If not, try to find out why. This will help you to modify the information you share and the way you share it. You may need to reinforce advice given by presenting it in different ways. Make sure that you and your colleagues are giving the same nutritional messages.
Figure 1. Demonstrating how to prepare a good meal
Adapting the guide:
makes the information relevant to local families and local nutrition problems;
provides an opportunity for nutritionists and others from different sectors and organizations to discuss the material and to update national or local nutrition guidelines. This process helps to create a sense of ownership of the guide.
Adaptation of the guide can be done at national or provincial level. People who might be able to help to prepare and produce a local version of the guide include:
staff from a regional nutrition institute or from departments of home economics or of food science and technology;
an experienced nutritionist, dietician and/or medical doctor who is familiar with the area and its problems;
staff from an appropriate United Nations agency, such as the Food and Agriculture Organization (FAO), the World Health Organization (WHO) and the United Nations Children’s Fund (UNICEF).
1. Before you and your colleagues adapt the guide you should discuss, find out and decide the following.
· Which ‘nutrition educators’ will use the guide. Will they be trained nurses and other health staff? Agricultural extension or other development workers? Community health workers? Leaders of community groups? Literate parents responsible for feeding the family? You need to know the level of knowledge and education of these educators so you make your guide relevant and easy for them to use. You may need to translate the adapted guide (or only the main messages) into the local language. You also need to know in which situations the guide will be used and what other learning/teaching materials the educators have.
· The characteristics of families with whom you or other educators will work. You need to know:
- what foods are available and eaten at different seasons; what the local feeding practices, knowledge and beliefs are; what local recipes are used; how food is shared among family members; how babies, young children, older children, women, men and old people are fed; what resources are available (e.g. land, money, water, time); how food is produced, stored, preserved and cooked; what the levels of hygiene are; which foods are eaten outside the home and by whom; who makes decisions related to family feeding;
- what types of nutrition problems and malnutrition are found in these families; which family members are at risk and what the probable causes are; what peoples’ perceptions and beliefs are, as well as their explanations about nutritional disorders and their causes (see Section C).
2. Decide which parts in the original guide to alter or delete, and what information to add.You will probably want to make changes to or add information on:
the feeding problems and types of malnutrition found locally;
foods suggested for healthy, balanced diets, adding important local foods that are not mentioned in the guide;
words used for foods, recipes, measures of weight and volume, etc., using local words;
methods used to increase food production;
varieties of legumes, vegetables and fruits to grow and animals and fish to raise;
methods used to store and preserve food, mentioning practices that can contaminate and/or waste food and making suggestions for improved practices;
ways used to preserve nutrients during cooking, emphasizing local methods that should be encouraged and pointing out those that decrease nutrient values;
advice on budgeting and ‘good buys’;
local recipes for feeding young children and sick people;
food composition tables, trying to use local ones;
sources of more information;
illustrations, making sure that any changes or additions are culturally as well as technically correct.
3. Prepare the revised guide. Do not make it too long and only include information that educators need to help families have good, balanced diets.
4. Field-test the guide with some educators and target families. Is the information practical as well as technically and culturally correct? Is the advice feasible for the different types of families you want to reach? Do the educators understand the text, concepts and illustrations? Is your guide easy to read and use?
5. If changes are still necessary, revise the guide, test it again and then prepare a final version.
(also see Topic 11)
People who have poor diets and do not eat the right amounts of energy-rich food and nutrients are often sick and become malnourished. The type of malnutrition that occurs depends on which nutrients and how much of the required food energy are lacking (or are in excess) and for how long, and the age of the person.
1. Children and adults may eat too little food and become undernourished because they do not have enough food or they have a poor appetite. These people lack energy and many nutrients, which means:
they have less energy so they cannot work, study or play as normal;
their immune systems are weak so they become ill easily and/or are seriously ill;
children stop growing and may lose weight. If very little food is eaten (often because of infection), a child may develop severe malnutrition (i.e. kwashiorkor or marasmus);
adults lose weight. If a pregnant woman is undernourished, her unborn baby grows poorly.
2. People may eat unbalanced diets that provide too little of a particular nutrient. For example:
if there is a lack of iron, the mental and physical development of children may be delayed. People of all ages are less active, have less immunity to infections and may become anaemic. Anaemic women have an increased risk of dying during and after pregnancy;
if there is a lack of iodine, people become more apathetic and find it hard to work or study. Sometimes a goitre develops. A woman who lacks iodine in early pregnancy is at high risk of having a child who is mentally and physically damaged. For example, the child may have a lower IQ or be deaf;
if there is a lack of vitamin A, people are more likely to become sick because the immune system is damaged. In severe vitamin A deficiency, there are eye conditions that range from night blindness to dry eyes (xerophthalmia), to corneal damage and blindness. These eye conditions occur most often in young children and pregnant women.
3. People may eat more food (especially energy-rich foods with plenty of fat and/or oil) than they need. By taking in too much energy they become too fat (overweight or obese). These people are at increased risk of chronic conditions, such as heart disease, high blood pressure and diabetes (see “Overweight and obesity”, page 14).
Malnutrition (due to both lack and excess of food energy and/or nutrients) is one of the biggest health problems in the world, especially in developing countries.
More than half the deaths of children aged 0-5 years are associated with undernutrition.
In many countries a third of the young children are stunted and 10 percent are too thin (wasted).
About a sixth of newborns have low birthweights, which makes them more likely to become ill, grow slowly and die.
Anaemia caused by lack of iron is the biggest nutrition disorder. In many places half the women are anaemic.
Vitamin A, iodine and zinc deficiency disorders are widespread in many countries.
Overweight and obesity and their related disorders are on the increase in most countries (see “Overweight and obesity”, page 14).
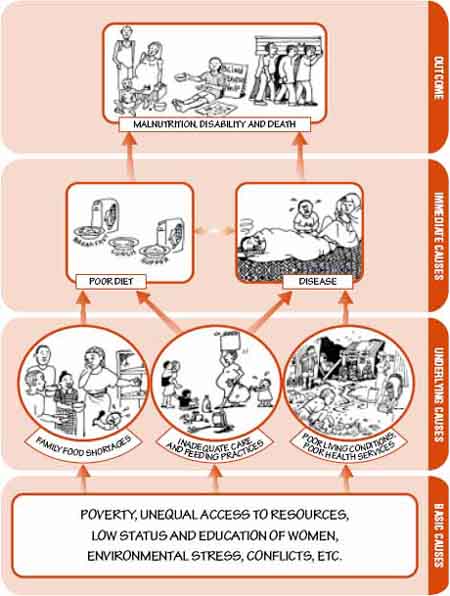
There are many reasons why a child or adult becomes undernourished. The causes vary from person to person but we can divide them into immediate, underlying and basic causes.
Immediate causes
These are a poor diet and disease.
A poor diet may be due to:
- insufficient breastmilk;
- meals that are too small;
- poor variety of food;
- low concentrations of energy and nutrients in meals (i.e. food is too ‘watery’);
- infrequent meals.
Disease. Sick people may:
- not eat much;
- absorb few nutrients;
- lose nutrients from the body;
- use up nutrients in the body more quickly (e.g. during fever).
Underlying causes
These include family food shortages, inadequate care and feeding practices, especially of children and women, and poor living conditions and poor health services.
Family food shortages, which may be due to:
- lack of money for food;
- low production of family food;
- poor food storage and preservation;
- poor choices and budgeting.
Inadequate care and feeding practices:
- the way families feed young children and encourage them to eat;
- the way families care for women (especially during pregnancy, childbirth and breastfeeding) and for sick and old people;
- the way food is prepared and the level of hygiene in the home;
- the ways families prevent and treat illnesses at home and use health facilities.
Poor living conditions (e.g. insufficient water, inadequate sanitation and overcrowded housing) and poor health services. Shortages of medicines and skilled health staff increase the risk of disease. Inadequate environmental sanitation services increase the risk of food-borne infections.
The role of women in food production, trade and preparation is vital but is often overlooked when causes of malnutrition are analysed and nutrition programmes are planned. In many countries, women produce much or most of the food. The level of care and quality of diet that women can give their families (including themselves) depends largely on their workloads and their social role within the family. For example, when women have heavy workloads (which many do), they may not have time to prepare more than one meal a day (which is especially insufficient for young children). If women have little authority and little control over resources (e.g. land, money), this also affects the type of care they can give different family members.Women’s workloads and social roles can be important underlying causes of malnutrition.
Basic causes
For each underlying cause there are ‘deeper’ causes. These may include:
widespread poverty and lack of employment opportunities;
unequal distribution and control of resources at community, district, country and international levels;
the low status and education of women;
population pressures;
environmental damage;
political unrest and conflict;
lack of health, education, and other social services;
discrimination.
Figure 2 on the opposite page demonstrates many of the different factors at various levels of society that can lead to malnutrition. Of course, these factors are more complicated in real life. In fact, malnutrition itself can reduce the ability of a family to care for all its members - and so creates a vicious circle of malnutrition and its underlying causes. For example, this happens when a malnourished child needs more attention from caregivers and hence further weakens the family's capacity to look after the needs (food, health, etc.) of other family members. The series of illustrations in Figure 2, nevertheless, helps us to identify the most important reasons why a person, family or community can be malnourished.
Box 3 below shows how HIV/AIDS is both an immediate and underlying cause of malnutrition (also see Topic 10, page 84).
BOX 3 · HOW HIV/AIDS CAUSES MALNUTRITION
|
HIV/AIDS can be an immediate cause of malnutrition because:
HIV/AIDS can be an underlying cause of food insecurity and malnutrition if:
Children often become malnourished if one or more parents is sick or dead. They may lack food and care, or they may eat less because of grief and depression. |
Adapted from the UNICEF Framework of Underlying Causes of Malnutrition and Mortality
Figure 2. Immediate, underlying and basic causes of malnutrition
Overweight and obesity
Overweight and obesity are principally caused by regularly:
eating too much food, particulary energy-rich food (often containing large amounts of fat and sugar);
having a lifestyle (work, sports, travel) that does not involve enough physical activity.
Obesity is now a worldwide epidemic. More than 1 billion adults are overweight and at least 300 million adults are obese (see Glossary for definitions of overweight and obesity). Overweight and obesity affect almost all ages and socio-economic groups, and the increasing numbers of obese children is a major cause for concern. In many developed and developing countries the obese proportion of the population has increased threefold since 1980. And this increase is often faster in developing countries than in developed ones. In most developing countries obesity and undernutrition are now major problems.
The increase in obesity is one of the main reasons for the increase in dietrelated chronic disease and disability.
The non-fatal, but debilitating health problems linked to obesity include respiratory difficulties, chronic musculoskeletal problems, skin problems and infertility.
The life-threatening problems are cardiovascular diseases, including hypertension and stroke, type 2 diabetes, certain types of cancers, and gallbladder disease.
The health consequences of these conditions range from premature death to disabilities that reduce the quality of life.